
|
|
|||||
|
|
|
|
|
|
|
![]()
Introduction
PACES stands for Practical Assessment of Clinical Examination Skills
Before candidates can enter the MRCP(UK) Part 2 Clinical Examination (PACES), they must have fullfilled the following criteria:
-
Passed the MRCP(UK) Part 2 Written Examination (or have been awarded exemption)
-
Completed a minimum period of training of two and a half years from the date of graduation given on their diploma of medical qualification.
-
Not less than 12 months should have been spent in posts involving the care of emergency medical patients, either adults or children
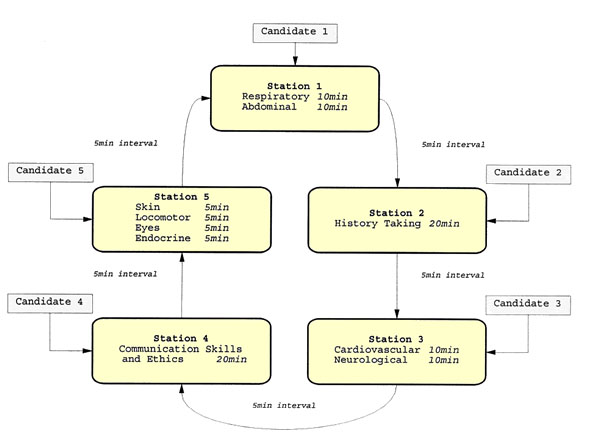
The process of this examination is best summarized by this image from Royal College MRCP website. Candidates going for station 2 and 4 must remember that they need to use the 5 min interval to read through the question and prepare for the respective station. To learn more about the exam, go to http://www.mrcpuk.org/PACES/
General Tips About MRCP PACES
MRCP Station 1
Examination of the respiratory system
-insufficient time spent on inpection,missing scar and abnormalities of shape and movement of chest wall.
- failing to percuss and auscultate over the apices and /or right down to the lung bases.
-not knowing normal leves of diapragm anteriorly and posteriorly.
-failing to assess tracheal position.
-failing to test vocal resonance.
-failing to consider non-respiratory disease (eg cardiac failure,nephroyic syndrome) in the differential diagnosis.
-inventing signs to fit a diagnosis.
Examination of the abdomen
-being too rough and causing the patient discomfort.
-not performing light palpation first.
-not ensuring patients breathe through their mouth when testing for downward organ movement
-failing to palpate for kidneys.
-failing to examine correctly for th presence of ascites.
-inventing signs.
MRCP Station 3
Examination of Cardiovascular system
-insufficient time spent on inspection, missing scars and abdominal pulsations.
-not adequately assessing character of heart sounds as well as murmurs.
- failing to turn patient to left lateral position and localize apex beat before listening to apex for MDM.
-failing to position patient correctly to examine for an EDM at the lower left sternal edge.
-FAILING TO ANALYSE MURMURS IN CONJUCTION WITH THE OTHER FINDINGS EG PULSE,POSITION OF APEX BEAT, ABNORMAL HEAVES AND HEART SOUNDS.
-not assesing JVP correctly, most commonly due to poor positioning of patient.
-inventing murmurs.
Examination of the CNS
-being too rough and causing patient discomfort.
-failing to instruct patient adequately, leading to wrong interpreattion of signs, especially when testing power, sensation and co-ordination.
-not taking into account patient's mental state and alertness.
-failing to assess gait, where approriate.
-failing to assess limb posture and muscle wasting/tone.
-failing to assess visual acuity and fields.
-performing an unstructured examination, especially when testing sensation.
-misinterpreting weakness as a cerebellar deficit when testing for co-ordination.
-poor and unpractised tendon hammer technique.
-failing to identify and intepret patterns of abnormalities.
-failing to recognise that not all neurological pathologies always present with absolutely typical features (eg UMN lesions may sometimes not be accompanied by increased tone and hyper-reflexia.)
-inventing signs.
MRCP Station 5
Examination of fundi
-insufficient practice with opthalmoscope.
-failing to assess for presence of cataracts.
-not describing what you actually see.
-inventing findings to fit pre-conceived diagnosis.
Examination of skin
-not describing what actually you see.
-guessing when you do not know the diagnosis.
Examination of Locomotor
-failing to establish whether the patient has active arthritis, with painful joints.
-being too rough and causing patient discomfort.
-poor assessment of joint movement, especially the spine.
-poor assessment of functional limitation, especially when examining the hands.
-inadequate knowledge of the differentiating feature between common arthropathies.
Examination of the Endocrine
-poor understanding of the patho-physiology of the common endocrine conditions.
-inadequate assessment of thyroid status and expecting patient to have active thyrotoxicosis if they have other features of Grave disease.
-poor assessment of dysthyroid eye disease
The Marking Of The MRCP(UK) Part 2 Clinical Examination(PACES)
The overall PACES score:
Fourteen mark-sheets in total are completed by the Examiners: two by each examiner at Stations 1 and 3; one by each Examiner at Stations 2,4 and 5. The Station Mark awarded on all fourteen mark-sheets determines the candidate’s overall PACES score.
All marks are recorded using a four-point grading system. These are
| Grade | Station Mark |
Clear fail |
1 |
Fail |
2 |
Pass |
3 |
Clear pass |
4 |
PACES is marked out of a total of 56 marks ( being the maximum available from the fourteen mark-sheets). A candidate will not pass if awarded three or more ‘clear fail’ grades regardless of the PACES score achieved. The nominal Pass Mark for PACES is 42. However, the MRCP(UK) Clinical Board has the authority to vary the Pass Mark.
How Do They Mark You?
|
CLEAR PASS |
PASS |
FAIL |
CLEAR FAIL |
System of Examination |
Examines thoroughly and systematically |
Examines systematically |
Examines inadequately, either by omission or by lack of system |
Examines badly and unsystematically |
Language and Communication Skills |
Talks to patient in a structured but flexible manner, using intelligible language and avoiding jargon. |
Talks to patient in a mainly structured manner. |
Uses unstructured language and is unaware of communication problems with the patient. |
Talks to the patient in a completely unstructured way and uses technical jargon. |
Confidence and Rapport |
Displays confidence, rapport and empathy. |
Demonstrates correct approach to the patient. |
May appear inappropriately confident, or unconfident/hesitant. Poor rapport with the patient. |
Causes the patient visible physical or mental distress and is oblivious to it. |
Clinical Method |
Demonstrates correct and comprehensive clinical method and skills, eliciting the correct physical signs. |
Demonstrates majority of clinical skills correctly and elicits the majority of physical signs correctly. |
Misses important or obvious physical signs, resulting in poor or incorrect formulation of differential diagnosis. |
Misses or invents the majority of physical signs and is unable to appreciate their significance in solving clinical problems. |
Discussion and Appreciation of Patient's Concerns |
Discusses clinical issues sensibly, spontaneously and with confidence, whilst able to negotiate and acknowledge areas of doubt/ignorance. Shows awareness of patient concerns. |
Majority of discussion sensible and correct, with no important errors of fact or interpretation. |
Inadequate appreciation of patient's problems and concerns. Large part of discussion incorrect through inadequate clinical skills or underlying ignorance. Is unaware of patient's concerns or deals with them inappropriately. |
Demonstrates an inability to discuss, or most of the discussion is incorrect, despite examiner's attempts at assistance. Lacks insight. |
Clinical Thinking |
Clear, appropriate and professional. Able to solve the problem posed by the patient. |
Reasonable clinical thinking. Muddled clinical thinking. |
Examiner has to work hard to give assistance. |
Poor grasp of clinical concepts and may be argumentative. |